Corey Diamond, PharmD
It may surprise some pharmacists that the practice of using vancomycin loading doses is not currently supported by robust clinical evidence. A 2020 consensus guideline from the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists has graded the current evidence with a B-II, which indicates a recommendation neither for nor against the practice. And while many institutional protocols recommend vancomycin loading doses of 20 mg/kg to 35 mg/kg to prevent treatment failure by rapidly reaching therapeutic concentrations, a new study published in the March 2021 issue of Therapeutic Advances in Infectious Disease suggests it may not matter.
Flannery and colleagues conducted a retrospective, single-center, cohort study that analyzed hard, clinical outcome data from more than 400 ICU patients—making it the largest study of vancomycin loading doses to date in any patient population with a protocol that adheres most closely with the 2020 consensus guidelines. The researchers stratified patients receiving vancomycin into two groups: patients who received a targeted loading dose of 30 mg/kg and those who received a targeted maintenance dose of 15 mg/kg upon therapy initiation.
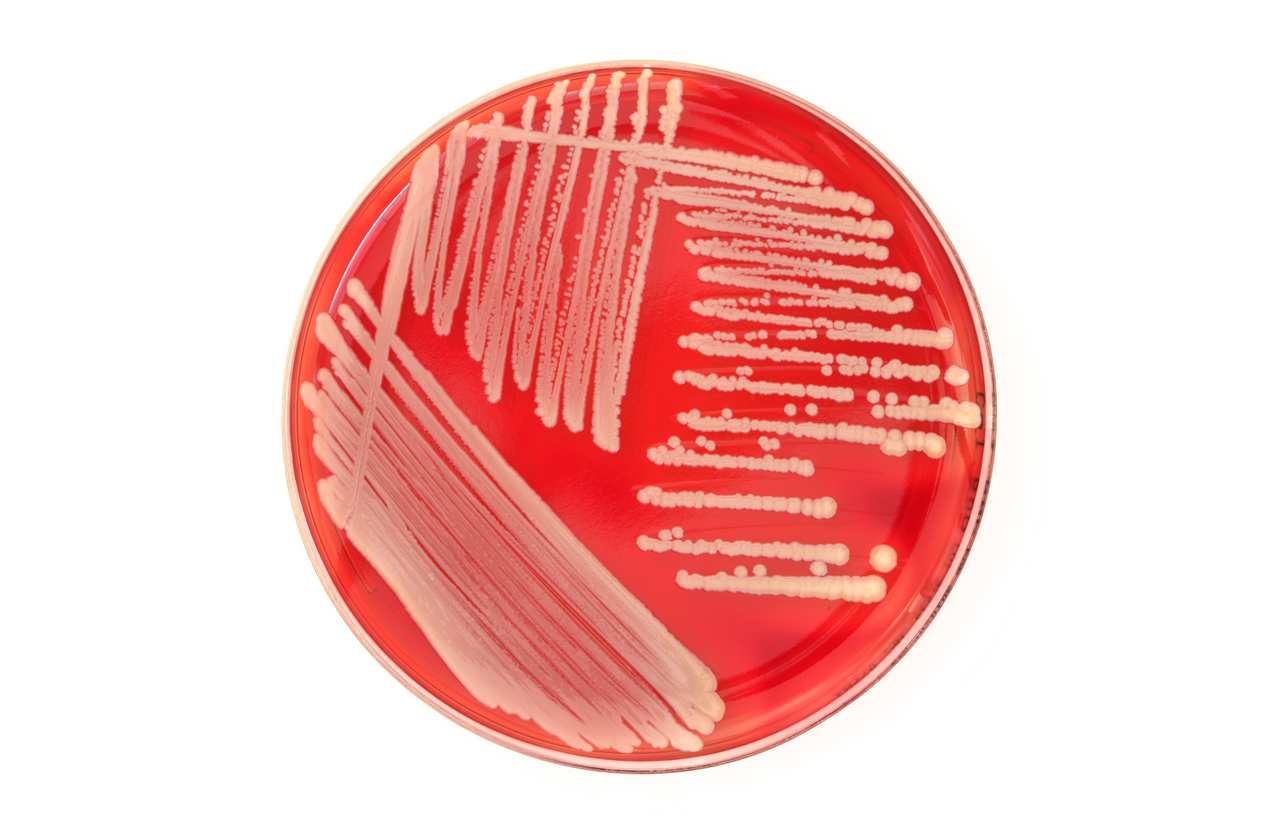
The researchers found no significant difference between the treatment groups in the primary outcome of clinical failure, which included a composite outcome of death within 30 days of first methicillin-resistant Staphylococcus aureus (MRSA) culture, blood cultures positive for more than 7 days, white blood cell count or temperature elevated more than 5 days after vancomycin initiation, or substitution—or addition—of another MRSA agent.
In addition, they detected no differences in any single component of the composite outcome, all-cause ICU mortality, acute kidney injury, or duration of vasopressor or mechanical ventilatory support.
More curious findings
There are, arguably, only four fully published studies in the literature that investigate the effect of vancomycin loading doses on a primary clinical efficacy endpoint; however, none are randomized controlled trials.
One study abstract published in the January 2021 supplement of Critical Care Medicine found similar results to those reported by Flannery and colleagues. In a retrospective, single-
center cohort study, Malaria and colleagues compared MRSA bacteremia cohorts given a median vancomycin dose of 26 mg/kg versus 16 mg/kg. Over a 7-day period, the researchers found no significant difference in their primary composite outcome that reflected clinical failure.
Another study worth mentioning was published in the Journal of Chemotherapy in 2018 by Weslock and colleagues. In contrast to the Malaria and Flannery studies, this retrospective cohort study’s primary efficacy outcome—time to systemic inflammatory response syndrome resolution—was statistically significantly less in patients with MRSA bacteremia who received a loading dose of 20 mg/kg or higher, compared with the control cohort. However, the researchers did not find a significant difference in mortality, time to negative blood cultures, or length of stay.
Most of the literature on this practice consists of small or low-quality observational studies that are relatively heterogeneic and have insufficient power to detect clinical outcomes. The studies that do have acceptable quality mainly contain objectives focused on achieving targeted therapeutic trough concentrations rather than clinical objectives.
On the flip side
In 2014, Kalil and colleagues published a landmark study in JAMA that demonstrated, among other things, that patients with MRSA bacteremia have an increased risk of mortality and prolonged hospitalization that is independently associated with delayed initiation of antimicrobials.
Particularly in patients with sepsis, each hour of delay in administering antibiotics, in general, is associated with a 7.6% reduction in survival.
This risk appears to put the 2020 consensus guideline into perspective. The guideline recommends considering the use of vancomycin loading doses only in patients with critical illness or chronic kidney disease that requires dialysis.
Coupled with what appears—at this juncture—to be a minimal effect on nephrotoxicity incidence, this makes the recommendation seem reasonable.
Ultimately, the current lack of power in the literature brings with it considerable empowerment for clinical pharmacists to use their judgment to mitigate vancomycin risk for their patients.
Hospitalists should review the literature themselves and reach their own conclusions about how to improve patient outcomes.