Loren Bonner & Clarissa Chan, PharmD

Hormone therapy, specifically estradiol and testosterone, are familiar drugs. Pharmacists know how they interact with other medications. What is less clear is how pharmacists fit into the changing landscape of clinics and health care teams as transgender individuals seek gender-affirming hormone therapy, a medical intervention to align appearance with gender identity.
“Gender-affirming hormone therapy dates back decades, but is a domain more providers are going to need to familiarize themselves with as it escalates in practice,” said Elisa Stanger, PharmD, a primary care clinical pharmacist from Cleveland Clinic’s Department of Pharmacy.
Stanger led a research study that showed exactly how clinical pharmacists could fit into the workflow of gender-affirming care for gender diverse patients in a community ambulatory setting.
At Cleveland Clinic’s Center for LGBTQ+ Care, the medical director and the institution’s primary care pharmacists worked to update their CPA to include gender-affirming hormone therapy when patients come in for routine gender-affirming hormone therapy follow-up.
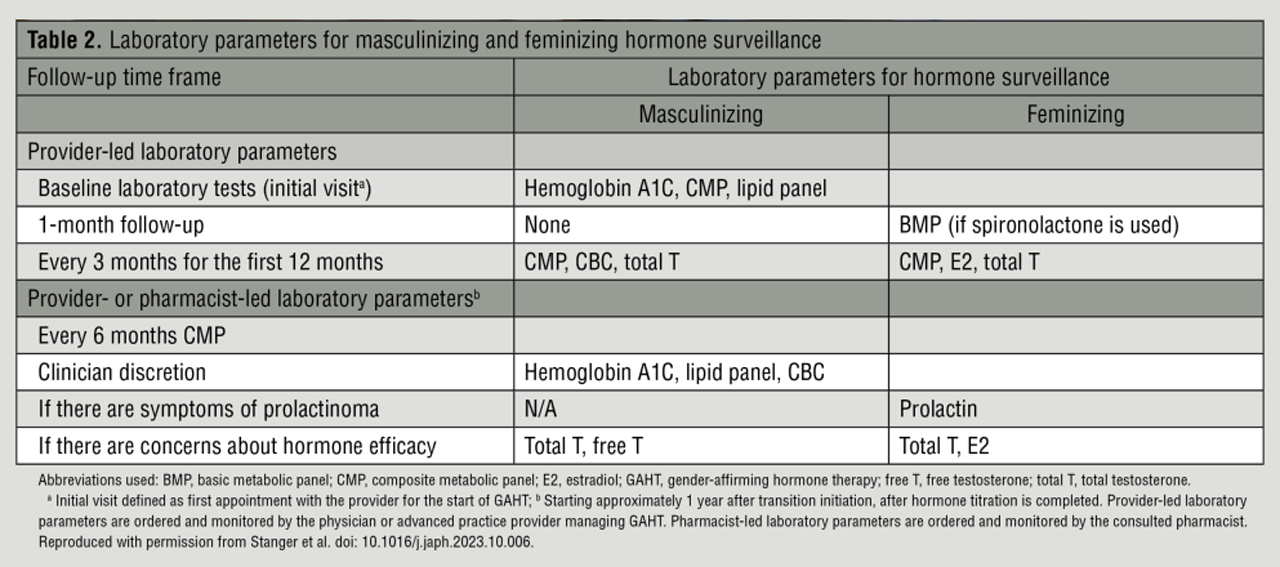
The study, published in the January/February 2024 issue of JAPhA, details the protocol the clinic used when a pharmacist managed gender-affirming hormone therapy for stable patients after they completed hormone titration provided by a physician or an advanced practice provider. In Ohio, pharmacists practicing under a CPA with a physician or other health care provider are allowed to order laboratory tests for patients and then modify drug therapy on the basis of those test results.
“We’ve seen published literature with pharmacists on these types of care teams,” said Stanger. “We feel we are showing where pharmacists can exactly fit into the workflow through a concrete protocol.”
In the updated CPA at Cleveland Clinic’s Center for LGBTQ+ Care, pharmacists can perform services to manage transgender care and gender transition as a primary diagnosis. Comorbid conditions that were elected to be included within the CPA update were hyperlipidemia/statin management, diabetes, smoking cessation, and hypertension.
“These comorbid conditions were specifically chosen given that they can develop or worsen with long-term hormone therapy and are imperative to monitor and treat accordingly,” wrote researchers.
At the clinic, pharmacists only see patients already established on gender-affirming hormone therapy for at least 6 months, at least 1 year after transition, and with a primary care provider managing their gender-affirming hormone therapy.
In the CPA, pharmacists can manage both feminizing (i.e., estrogens, antiandrogens, and progesterone) and masculinizing (i.e., testosterone and a-alpha reductase inhibitors) hormone therapy.
Testosterone levels were included for masculinizing hormone surveillance. Similarly, estradiol levels and testosterone levels were included for feminizing hormone surveillance if there were any concerns about hormone efficacy.
Given that elevations in liver enzymes can occur with testosterone, estrogen, and cyproterone acetate, pharmacists at the clinic are able to order a complete metabolic lab panel for patients. They also monitor and assess serum potassium levels with the use of spironolactone; hematocrit and the risk of polycythemia with masculinizing hormone therapy; and prolactin and the risk of hyperprolactinemia for those taking estrogen therapy.
Given the increased risk of hyperlipidemia and diabetes with hormone use, clinical Cleveland Clinic pharmacists are able to order a lipid panel and A1C test. Stanger noted that the protocol is still fairly new at the clinic. Gender-affirming hormone therapy management was only approved to be added to the pharmacists’ CPA in May 2022. Pharmacists started seeing patients at Cleveland Clinic’s Center for LGBTQ+ Care in February 2023.
“This is only a brief report, there is more to come,” she said.
State level
Of course, a pharmacist’s ability to do any of this hinges on their state of practice—not only the state’s pharmacy scope of practice law, but also any laws pertaining to gender-affirming care, which can vary by state.
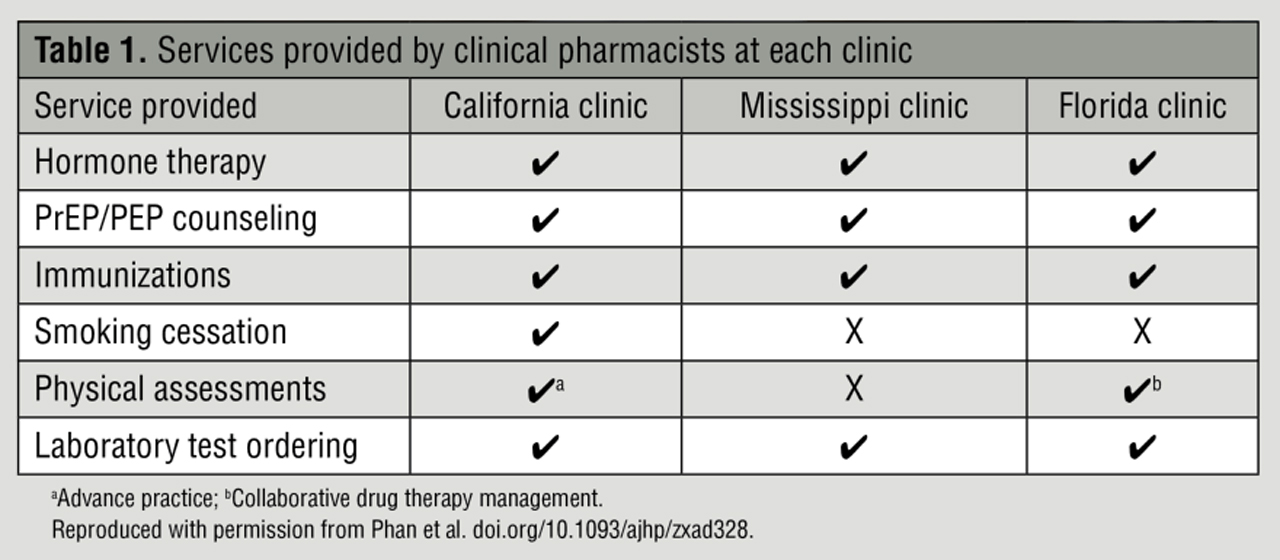
A report published on December 29, 2023, in the American Journal of Health-System Pharmacy explored how pharmacist-led services are integrated into practice in three states with varying legislation for sexual and gender minority populations.
Researchers looked at services in California, Mississippi, and Florida, specifically, in order to get a comprehensive view of the challenges—and opportunities—for putting pharmacist-led services into practice. These three states have different legislative and professional scopes for clinical pharmacists, and they are all culturally different as well.
“Our practice settings enable us to address a case that is as thought-provoking as it is interesting, allowing us to uncover real-world implications of pharmacist-led initiatives across different states and health systems,” said lead author of the study Tam Phan, PharmD, from the University of Southern California.
The services provided by clinical pharmacists at various sites in these states included gender-affirming hormone therapy management; HIV antiretroviral medication adherence programming; primary care and chronic disease state management; and involvement in care related to mental health, psychiatry, and substance use as well as sexual health services.
In Florida, for instance, pharmacists work in a sexual and gender minority health clinic network that has been designated as a federally qualified health center look-alike. Through a collaboration with a local college of pharmacy, clinical pharmacy services were offered to providers at all three clinic locations. Through the collaboration, providers determined that pharmacists would benefit patients and providers most with services focused on polypharmacy and appropriate medication use.
Pharmacy practice in Florida allows for an advanced scope of practice through the scope of collaborative drug therapy management. Legislation is currently progressing through the Florida legislature to expand existing “test to treat” CPAs to include HIV PrEP.
At all three clinics in these respective states, the lead pharmacists have worked with administrators to develop CPAs to expand the scope of practice for medication management services.
Given that many medications prescribed in gender-affirming care are used off-label, all three sites drew on available evidence-based guidelines to inform clinical decision-making, including, but not limited to, the World Professional Association for Transgender Health Standard of Care (version 8), the Endocrine Society clinical practice guideline, and guidelines from the UCSF Center of Excellence for Transgender Patients.
Phan said that notwithstanding the diversity of practice settings, there was a striking similarity in the services rendered by pharmacists.
“This phenomenon likely arises from a shared recognition among the [pharmacists] of various health disparities prevalent across various disease states, such as gender-affirming hormone therapy and HIV [antiretroviral drugs] adherence,” he said.
As the authors noted, putting these services into practice requires a thorough evaluation of legislative and regulatory barriers, the diversity of patients’ sociodemographic characteristics, and the systemwide scope of practice for pharmacists.
The report also focused on how pharmacist-led initiatives could enhance health outcomes and bridge health care gaps for sexual and gender minority populations.
“[Pharmacists] expertise proved essential in navigating intricate medication schedules, supporting adherence rates, and imparting knowledge on correct medication usage,” said Phan.
Sexual and gender minority populations also report negative experiences with health care providers, which keeps many away from seeking out health care in the first place.
Stanger said that some of their patients travel far distances to seek care at Cleveland Clinic’s Center for LGBTQ+ Care.
“Patients will post on Reddit and other social media platforms if they find a good [gender-affirming hormone therapy] provider—we found they did that with our Cleveland Clinic providers,” Stanger said.
Psychotropic medication interactions
Phan said their report also supports the need for pharmacists’ involvement in mental health care due to the higher risk of mental health conditions among sexual and gender minority individuals.
Research has shown that transgender people are at a greater risk of mental health conditions such as depression, anxiety, suicidal ideation and suicide attempts, and substance use.
Among transgender individuals who have access to medical care, emerging data suggest a high prevalence of psychotropic medication use.
According to a study published in the January/February 2024 issue of JAPhA, among more than 300 transgender peo-ple on gender-affirming hormone therapy, including either estradiol or testosterone therapy, more than half had at least one order for a psychotropic medication. Of this cohort of individuals, more than one-third were on two or more psychotropic medications with overlapping treatment durations.
For the authors of the study, it was clear that pharmacists can identify and address potential drug–-hormone interactions between hormone therapy and psychotropic medications—and they wanted to demonstrate that.
“Because potential drug–hormone interactions exist between certain psychotropic medications and gender-affirming hormone therapies, pharmacists may play an important role in identifying and managing drug therapy problems, including drug–hormone interactions, for transgender people,” said lead study author Lauren Cirrincione, PharmD, MPH, from the Department of Pharmacy at the University of Washington.
“Reassuringly, most types of psychotropic polypharmacy we observed in our analysis appeared to align with current mental health treatment guidelines,” she said. “However, the number of people with at least one potential drug–hormone interaction between psychotropic medications and concurrent hormone therapy was significantly higher among those with psychotropic polypharmacy.”
Cirrincione said their small hypothesis-generating analysis was designed to provide a better understanding of the patient-level psychotropic medication burden and potential drug therapy problems for transgender individuals on gender-affirming hormone therapy for future pharmacist-led interventions.
“Follow-up investigations, including prospective pharmacokinetic studies, are needed to characterize the potential drug–hormone interactions observed in this analysis,” Cirrincione said.
She added that not every transgender person wants or has access to medical care or gender-affirming hormone therapy.
“Given our focus on potential interactions with hormone therapy, our analysis was limited to transgender people on gender-affirming hormone therapy within a single health system,” she said. “Future investigations of psychotropic polypharmacy should consider characterizing the patient-level psychotropic medication burden for transgender people not on hormone therapy, and comparing the medication burden both before and during hormone therapy when possible.”
At Cleveland Clinic’s Center for LGBTQ+ Care, mental health conditions were not part of the CPA that could be managed directly by the pharmacist at the time of protocol development and therefore not included as comorbid conditions. The authors did, however, acknowledge how important mental health conditions are as they relate to gender-affirming care. ■

Pharmacists as champions in access to hormone therapy for transgender and gender-diverse individuals
One of the most powerful ways pharmacists can help facilitate access to gender-affirming hormone therapy is by being an advocate for gender-affirming care,” said Julianne Mercer, PharmD, pharmacotherapy resident at the University of Texas at Austin College of Pharmacy and University of Texas Health Science Center at San Antonio. WHO defines gender-affirming care as “a range of social, psychological, behavioral, and medical interventions designed to support and affirm an individual’s gender identity.”
Transgender and gender-diverse individuals face substantial health disparities, including an elevated susceptibility to self-harm, suicide, mental health challenges, and substance use compared to the general population.
Findings from a review published in the November/December 2023 issue of JAPhA can help pharmacists better understand gender-affirming hormone therapy (GAHT) and their related health concerns to help facilitate a patient’s access to GAHT, with emphasis on patient treatment goals, preferences, and tolerability in therapy choices.
“With the increase in legislation isolating this group and the prevalence of reported negative experiences in health care and other stress-inducing factors, we can identify these as potential elements contributing to the minority stress theory,” said Mercer, who was the lead author of the JAPhA review.
This theory suggests that negative social experiences such as isolation, stigma, and discrimination pose risks to a person’s physical and mental health outcomes.
“Therefore, advocating for equitable care and environments of belonging is crucial, impacting direct social experiences as well as potentially physical and mental health outcomes as well,” said Mercer.
Information to assess risks, benefits
Several of the links explored in the study—particularly in relation to CV and cancer risks—are inconclusive. They have not demonstrated much difference from that of cisgender counterparts, and need to be investigated further.
“Health care providers should still inform their patients that the risks associated with [feminizing hormone therapy] and [masculinizing hormone therapy] are not completely understood; most of what we know has been derived from trials conducted on cisgender individuals,” said Justina Lipscomb, PharmD, BCPS, clinical assistant professor at the University of Texas at Austin College of Pharmacy and University of Texas Health Science Center at San Antonio, University Health System, an author of the study.
The target ranges for serum estradiol and testosterone levels in transgender and gender-diverse patients taking GAHT are also based on reference ranges for sex hormones in cisgender patients.
However, dose adjustments should be made in accordance with each patient’s needs, goals, and safety, she said.
“A patient suffering from gender dysphoria may seek maximum hormonal therapy, while another patient may choose not to receive any hormone therapy,” said Lipscomb.
Although hormone therapy offers many benefits to patients, pharmacists must be aware of potential adverse effects, she said.
“For example, in individuals with testes, prolonged estrogen exposure may result in testicular atrophy,” said Lipscomb. “When estrogen therapy is discontinued, sperm production may not fully recover, reducing the possibility of conception.”
Before starting therapy, patients should be informed of the potential GAHT impacts on fertility, said Lipscomb.
“The benefits of gender-affirming care are best achieved after patients have expressed their goals and been provided with information to assess the risks and benefits,” she said. “Every patient should feel empowered to verbally express their needs and be permitted to seek the interventions, whether pharmacological or nonpharmacological, that affirm their gender identity.”
Role of pharmacists
As with any treatment, health care providers have a duty to communicate the risks of therapies and any knowledge gaps in existing literature. For GAHT in particular, the data on renal dosing, CV health, fertility, and cancer-related health outcomes are evolving.
“Existing data present conflicting information,” said Mercer. “Pharmacists should acknowledge that for many of these health risks, there are limited established causality explanations between appropriately managed GAHT and increased negative health outcomes.”
However, there are still risks associated with GAHT, that vary across drug doses and formulations, that should be communicated to providers and patients to ensure their safety and awareness of potential adverse outcomes, said Mercer.
“The most encompassing communication strategy involves acknowledging current research limitations studying long-term outcomes in this population, communicating patterns, and trends based on available data, and leveraging clinical judgment to educate based on a patient’s concomitant risk factors,” said Mercer.
Need for updated knowledge
While pharmacists are poised to offer guidance and education to patients and fellow health care providers concerning associated risks, many pharmacists feel ill-equipped to handle GAHT.
“It can be a challenge to locate comprehensive and accessible resources regarding GAHT post-pharmacy school,” said Lipscomb. “However, first-line resources include standards of care documents and guidelines like those produced by World Professional Association for Transgender Health (WPATH), UCSF Transgender Care, and the Endocrine Society.”
Podcasts and online videos covering topics on GAHT such as the ASHP Therapeutic Thursdays and the NIH virtual meeting on health disparities among sexual and gender minorities are also valuable resources, said Mercer.
Another strategy is to proactively create learning opportunities. “For instance, in a community pharmacy, a pharmacy leader could introduce readily available guides that provide resources for promoting inclusive care [such as Human Rights Campaign and APhA],” said Mercer.
Updated reviews of knowledge and strategies can empower pharmacists to deliver compassionate and well-informed patient care for individuals undergoing GAHT. ■