Simvastatin falls short in treatment of patients with Parkinson disease
Although current treatments for patients with Parkinson disease (PD) exist, there are no known treatments that slow disease progression. Preclinical and epidemiological studies support the potential use of statins as disease-modifying therapy, leading researchers from the PD STAT Study Group to investigate the efficacy of simvastatin to prevent clinical decline in patients with moderately severe Parkinson disease. The study was published in JAMA Neurology on October 31, 2022.
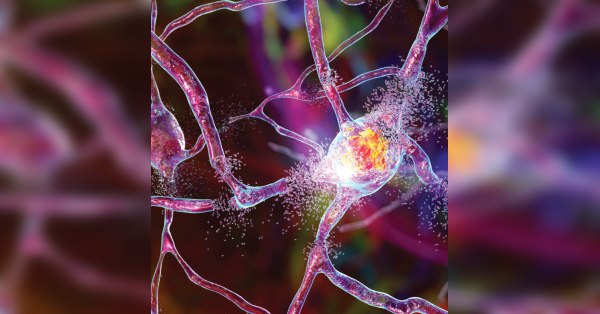
The randomized clinical trial, a double-blind, parallel-group, placebo-controlled futility trial, was conducted between March 2016 and May 2020 within 23 National Health Service Trusts in England. Participants aged 40 to 90 years with a diagnosis of idiopathic PD, with a modified Hoehn and Yahr stage of 3.0 or less while taking medication and taking dopaminergic medication with wearing-off phenomenon were included.
Participants were allocated 1:1 to simvastatin or matched placebo with patients in the simvastatin arm given 40 mg simvastatin daily for one month, followed by 23 months of 80 mg simvastatin daily and a 2-month washout period. The primary outcome was 24-month change in Movement Disorder Society Unified Parkinson Disease Rating Scale part III score measured while not taking medication,
Participants in the simvastatin group had an additional deterioration in Movement Disorder Society Unified Parkinson Disease Rating Scale part III scores while not taking medication compared with compared with the placebo group. The number of serious adverse events was similar in both groups.
The authors concluded that simvastatin was futile as a disease-modifying therapy in patients with moderately severe PD, providing no evidence to support proceeding to a Phase 3 trial.
Cefepime/enmetazobactam may improve treatment for complicated UTI
Complicated UTIs are one of the most common causes of sepsis in hospitalized patients. While a simple UTI typically responds to antibiotic treatment within 24 to 48 hours, a complicated UTI doesn't respond to a single course of antibiotic treatment. These complicated UTIs often require treatment with broad-spectrum antibiotics. In a paper published in the October 4, 2022, issue of JAMA, Kaye and colleagues investigated the efficacy of cefepime/enmetazobactam, a novel β-lactam/β-lactamase inhibitor combination, compared with piperacillin/tazobactam for the treatment of complicated UTI or acute pyelonephritis (a complication in which the infection spreads to the kidneys). The researchers conducted a phase 3, randomized, double-blind, noninferiority clinical trial at 90 sites in Europe; North, Central, and South America; and South Africa.
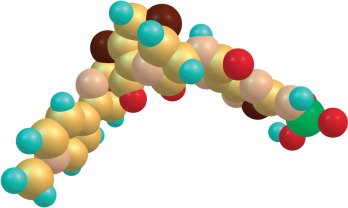
Over 1,000 adult patients with a clinical diagnosis of complicated UTI or acute pyelonephritis caused by gram-negative urinary pathogens were randomized to receive either 2 g cefepime/0.5 g enmetazobactam or 4 g piperacillin/0.5 g tazobactam, by 2-hour infusion every 8 hours for 7 days (or up to 14 days in patients with a positive blood culture at baseline). The primary outcome was the proportion of patients who achieved overall treatment success, defined as clinical cure combined with microbiological eradication (< 103 CFU/mL in urine). This primary outcome occurred in 79.1% of patients receiving cefepime/enmetazobactam compared with 58.9% of patients receiving piperacillin/tazobactam. Treatment-emergent adverse events occurred in 50.0% of patients treated with cefepime/enmetazobactam and 44.0% of patients treated with piperacillin/tazobactam. Most adverse events were mild to moderate in severity. The authors note that further research is needed to determine the potential role for cefepime/enmetazobactam in the treatment of complicated UTI and pyelonephritis.

Does chronic medication use affect risk of COVID-19 death in hospitalized patients?
Among the questions raised during the pandemic is the potential association between chronic medication use and death due to COVID-19. Researchers from the Vall d'Hebron University Hospital (Barcelona) used a retrospective cross-sectional study to investigate the relationship between the use of various medications and the seriousness of COVID-19 infection. The study, published on October 27, 2022, in the European Journal of Hospital Pharmacy included 978 patients hospitalized due to COVID-19 early in the pandemic. Of these patients, 4.2% were smokers, 16.7% were obese, 47.4% had hypertension, and 19.4% were diabetic; 182 patients died during the study follow up. Most patients (70.8%) were prescribed at least one medication, 32.5% used more than 5 medications, and 8.6% were prescribed more than 10 medications. The study results suggest that hospitalized COVID-19 patients taking trimethoprim and analogues, leukotriene receptor antagonists, calcineurin inhibitors, aldosterone antagonists, selective immunosuppressants, propulsives, insulins and analogues, and benzodiazepine derivatives have a higher risk of death from COVID-19. The authors note that further research is needed to increase understanding of the impact of chronic medication use to increase understanding of the relevance of their results.
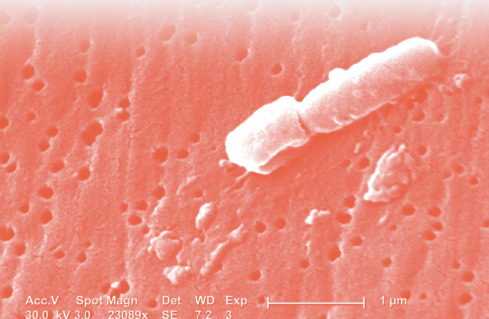
Carbapenem-resistant Klebsiella Pneumoniae growing in U.S. hospitals
Carbapenem-resistant Enterobacterales, those that are either resistant to carbepenum antibiotics or contain a carbapenemase that make the antibiotic ineffective, are spreading within the U.S. hospital system. The genes responsible for carbapenemase production are often on mobile genetic elements, which can be easily shared between bacteria, leading to the rapid spread of resistance. A recent study by van Duin and members of the Multi-Drug Resistant Organism Network Investigators Network Investigators and the Antibacterial Resistance Leadership Group published on September 29, 2022, in Clinical Infectious Diseases evaluated the spread of carbapenem-resistant Klebsiella pneumoniae (CRKp), the most prevalent carbapenem-resistant Enterobacterales in the United States. The study cohort consisted of 350 hospitalized patients with a single, positive culture for CG258 K. pneumoniae across 25 U.S. healthcare systems (with 42 hospitals) in 13 states and the District of Columbia from the Consortium on Resistance Against Carbapenems in Klebsiella and other Enterobacterales (CRACKLE-2) study. The researchers evaluated samples from these hospitalized patients to better understand clustering in CRKp isolates. Their results showed evidence of extensive nosocomial transmission and spread of CG258 CRKp in U.S. hospitals. Most patients had a CRKp isolate that could be genetically linked to an isolate of at least one other patient, regardless of the method used to assign clusters. Most patients were part of clusters with patients from the same health care system; however, about one-third of clusters showed evidence of transmission across health care systems. The authors note that the occurrence of intersystem clusters may indicate involvement of other health care sites (e.g., skilled nursing facilities and long-term acute care hospitals) as well as the community in perpetuating CRKp spread and emphasize that successful control of multidrug-resistant organisms requires infection prevention measures at both local and regional levels.